This is the incredible story of Linda, who will be celebrating her 27th Survivor Anniversary in 2020 after being given a diagnosis with a survival rate of less than 2 years.
The year is 1993 – the Internet is just at its dawn, spread of information is slow, scarce and with no particular focus on rare topics. A woman in her 30s from Big Springs, Kansas, USA, who is a mother of two young boys, enters Dr. Robert Dinsdale’s ENT specialist office in Lawrence, Kansas, to check on her child’s ear infection. Call it pure chance, a strong medical pro-active approach or a young doctor who remembers “when you hear hoofbeats, think Zebras”, but Dr. Dinsdale notices something unusual in this woman’s outward neck appearance and recommends that she has it checked out. She follows his advice and that saves her life.
This the beginning of Linda Mangelsdorf-Oshel’s NET cancer survival journey. It started with two months of testing, followed by a diagnosis of Stage IV Metastatic Familial Hereditary Bilateral Paraganglioma. Linda’s case was sent out to 5 top renowned head/neck cancer specialists from the KU Medical Center such as MD Anderson, The Mayo, John Hopkins, a well-known hospital in California, and to Rush -St Luke’s-Presbyterian Hospital in Chicago. Four of these top cancer places said they wouldn’t take the case as being too risky. Dr. William Panje at Rush-St. Luke’s- Presbyterian hospital in Chicago was the only one who considered doing the surgery as long as Linda knew she had less than a 10% chance of surviving the surgery and a 2-year post operation life expectancy. With that small of a chance, Linda packed her bags, headed to Chicago, and went off to surgery without telling her children where she was going or why as she felt they were too young to understand at ages 9 and 6. Dr. Panje saved her life. The surgery lasted about 14 hours. After surgery Linda was comatose for 5 days and in intensive care. On the fifth day Linda sat up in bed, to the doctor’s surprise, and was moved to a regular room.
Rush-St Luke’s-Presbyterian (the name of the hospital) was a teaching hospital and because Linda’s tumor was very, very rare Linda had about 14 interns studying the surgery, recovery, following the doctor around. She was told that the tumor was more involved than they thought and that 4 of her 12 cranial nerves had to be sacrificed in the surgery {lX, X, Xl, XIl), her left external carotid artery was removed; her vocal chords were separated and paralyzed and she was told that she would never have audible voice again, and because of the loss of cranial nerves that she would never swallow again and a feeding tube was permanently placed in her stomach. It was removed some 9 months later, when against all odds she taught herself to swallow and talk although with a slight post-operative British accent. Linda is a Native Kansan and this post-operative “accent” is referred to as Foreign Accent Syndrome (FAS) and she still has the accent to this day.
In 1993 Linda was working as an executive secretary to the President of a local corrugated box company. Eleven years later she decided she needed to “repay” for the care, inspiration and encouragement that she received from the nursing staff during her cancer surgery recovery and Linda went back to school at age 45, starting at page 1, became a registered nurse, and got her Bachelor’s in Nursing and a Certification Specialty in Rehabilitation Nursing.
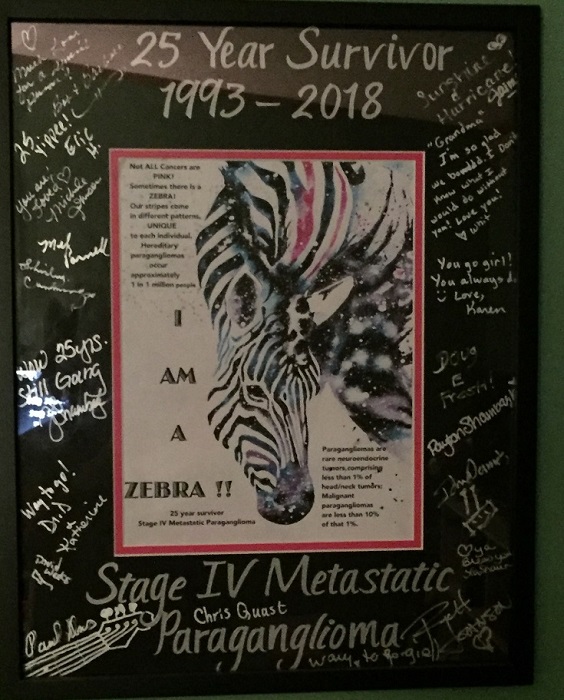
In 2018, Linda celebrated her 25th ZEBRA Survivor Anniversary!
Recently, she Facebook messaged us here at International Neuroendocrine Cancer Alliance
“I thought my pictures might give people an idea to celebrate their “ZEBRAness”!!! And if in sharing “my story”, I have touched a life (encouraged, inspired, helped), then my extra days of living granted by God’s Grace & Miracles and His hand in the skill of the surgeon that He led me to who saved my life, then I have not lived in vain” Linda Mangelsdorf-Oshel
More about paragangliomas and Linda’s input in research of the disease: The tumor is genetic, hereditary and is studied at many hospitals in the United States and in Europe. Linda participated in a genetic study from the University of Pittsburgh, Pennsylvania Cancer lnstitute (she also provided blood samples from her two sons). The genetic marker has been identified through the Human Genome project. The gene is a male dominant marker meaning usually the male carries the gene and passes it to his offspring. Females usually carry the gene and develop the tumor. Most of the tumors are benign or non-cancerous, however, Linda’s was stage lV terminal.
To learn more about paragangliomas visit the Pheo Para Alliance website.